A new wearable, noninvasive monitoring device prototype monitors glucose in sweat—no needles necessary.
Noninvasive glucose monitoring devices are not currently commercially available in the United States, so people with diabetes must collect blood samples or use sensors embedded under the skin to measure their blood sugar levels.
Now, with the new wearable device, less intrusive glucose monitoring could become the norm.
The researchers constructed the device first with laser-induced graphene (LIG), a material consisting of atom-thick carbon layers in various shapes. With high electrical conductivity and a convenient fabrication time of just seconds, LIG appeared to be an ideal framework for the sensing device—but there was a significant caveat.
“The challenge here is that LIG is not sensitive to glucose at all,” says Huanyu “Larry” Cheng, professor in Penn State’s engineering science and mechanics department. “So, we needed to deposit a glucose-sensitive material onto the LIG.”
The team chose nickel because of its robust glucose sensitivity, according to Cheng, and combined it with gold to lower potential risks of an allergic reaction. The researchers hypothesized that the LIG outfitted with the nickel-gold alloy would be able to detect low concentrations of glucose in sweat on the skin’s surface.
A material with high glucose sensitivity was a priority. Sweat exhibits remarkably low glucose concentrations compared to blood—but, according to Cheng, there is a strong correlation between glucose levels in sweat and blood. While the concentration of glucose in sweat is about 100 times less than the concentration in blood, the team’s device is sensitive enough to accurately measure the glucose in sweat and reflect the concentration in blood.
The nickel-gold alloy’s sensitivity allowed the researchers to exclude enzymes, which are often used to measure glucose in more invasive, commercially available devices or in noninvasive monitors proposed by other researchers. These enzymes, however, can degrade quickly with time and changing temperatures.
“An enzymatic sensor has to be kept at a certain temperature and pH, and the enzyme can’t be stored in the long term,” Cheng says. “A nonenzymatic glucose sensor, on the other hand, is advantageous in terms of stable performance and glucose sensitivity regardless of these changes.”
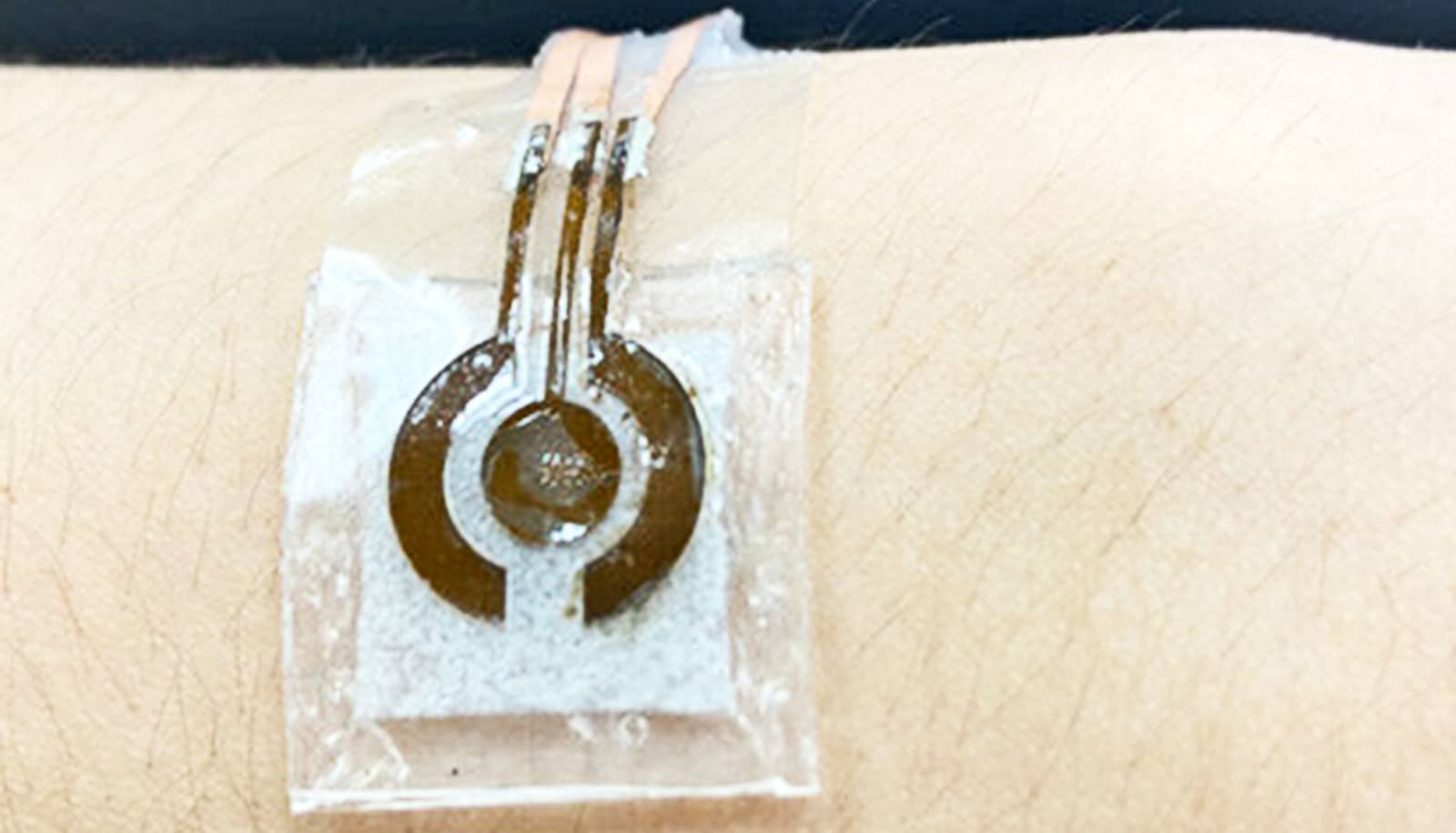
Nonenzymatic sensors require alkaline solution, which can damage the skin and typically limits device wearability. To curb this issue, Cheng and his team attached a microfluidic chamber to the LIG alloy. This chamber is smaller than previously developed configurations to promote wearability and porous to allow for a range of movement, such as stretching or crushing. It is connected to a collection inlet that passes sweat into the solution without allowing the solution to touch the skin. The basic solution interacts with the glucose molecules to produce a compound that reacts with the alloy. This reaction triggers an electrical signal, indicating the concentration of glucose in the sweat.
With a smaller alkaline solution chamber, the entire device is roughly the size of a quarter and is flexible enough to maintain a secure attachment to the human body, Cheng says.
In a proof-of-concept test, the researchers used a skin-safe adhesive to attach the reusable device to a person’s arm one hour and three hours after a meal. The subject performed a brief workout—just enough to produce sweat—right before each measurement time. A few minutes after collecting the sweat, the researchers found that the detected glucose concentration dropped from the first measurement to the next. The glucose measurements from the device were verified by measurements made with a commercially available glucose monitor.
The researchers plan to improve their prototype for future applications, including addressing how patients or clinicians may use the sensor for incremental glucose measurements or continuous monitoring to determine treatment actions, such as administering insulin.
They also intend to refine and expand this platform for more comfortable monitoring of other biomarkers that can be found in the sweat or interstitial fluids that fill the space between cells in the body.
“We want to work with physicians and other health care providers to see how we can apply this technology for daily monitoring of a patient,” Cheng says.
“This glucose sensor serves as a foundational example to show that we can improve the detection of biomarkers in sweat at extremely low concentrations.”
The research appears in Biosensors and Bioelectronics. Additional researchers are from Penn State and the Wuhan University of Technology in China.
The National Science Foundation and the National Heart, Lung and Blood Institute of the National Institutes of Health supported this work.
Source: Penn State